Bridging Eastern & Western Medicine
Discover How MBR Practitioners Can Alleviate Your Foot Pain

Check & See If Any of These are Applicable
Here are Potential Factors Contributing to Your Foot Pain

One leg feels long, or one side of the pants drags to the ground.
The pelvis feels asymmetric, or the pelvis touches the floor feels asymmetric when lying down.
After walking a lot, the skirt or pants turn to one side.
Feels limping when walking.
Even a little walk on the calf and feet feels tired.
The big toe is deformed, and calluses often form on the soles of the feet.
Toes are tingling and sore.
Prone to have an ankle sprain.
Common Foot Disorders
Achilles Tendinitis
Step-by-Step
Types of Foot Pain
Type 1. Plantar Fasciitis
What is plantar fasciitis?
The plantar fascia is a thick band of tissue that spans the underside of the foot, connecting the heel bone to the toes. Its primary function is to support the foot arch, distributing weight and mitigating shock. The most common symptom of plantar fasciitis is a sharp, stabbing pain experienced during the first steps taken in the morning. If left untreated, this condition can become chronic, causing ongoing heel or foot pain with each step.
What are the causes of plantar fasciitis?
When the foot possesses a normal arch, it effectively distributes weight and absorbs shock while walking. However, if the foot has a low arch, its ability to distribute weight and absorb shock is compromised. Excessive tension and stress on the plantar fascia can lead to the development of small tears in the tissue. The repeated stretching and tearing can result in irritation and inflammation of the fascia. Several factors contribute to this condition, including sudden or strenuous exercise, prolonged periods of standing, rapid weight gain, and fatigue.
What are the symptoms of plantar fasciitis?
Worst pain experienced during the initial steps after waking up in the morning.
A sharp pain on the heel side when getting up after prolonged periods of sitting
Stiffness and intensified pain when standing for extended periods.
Increased pain during dorsiflexion (pulling the toes upward).
How can orthotics help in the treatment of plantar fasciitis?
Foot orthotics play a significant role in the treatment of plantar fasciitis, particularly when the foot arch is collapsed or flat. However, if the individual has a normal foot arch, treatment can be pursued without the use of orthotics. Generally, through EMS pain treatment, more than 90% of patients experience symptom improvement within 6 to 8 weeks.
Type 2. Bunion
A bunion is primarily caused by a low foot arch, which affects the distribution of weight and the foot’s ability to absorb shock while walking. This condition leads to the deformation of the big toe.
What are the symptoms of a bunion?
The big toe pushes against the adjacent toe, typically the index toe.
The first metatarsophalangeal (MTP) joint turns outward (or medially), causing the big toe to point in the opposite direction. This can result in redness, friction with shoes, the formation of calluses, inflammation, and pain.
The weakened strength of the big toe affects the gait, causing fatigue in the feet and legs and potentially leading to lower back pain.
What angle between the 1st metatarsal and the proximal phalanx determines the severity of a bunion?
Mild
Angle <20 degrees, with an intermetatarsal angle usually less than 11 degrees.
Moderate
Angle between 20 and 40 degrees, with the intermetatarsal angle ranging from 11 to 18 degrees.
Severe
Angle > 40 degrees, with an intermetatarsal angle exceeding 16 to 18 degrees.
Can a bunion occur even if you don’t wear high heels or narrow shoes?
Yes, even without wearing high heels or narrow shoes, a bunion can develop. This is particularly true for individuals with low foot arches or flat feet. In such cases, the propulsion of the big toe is weak, leading to a gait pattern with the toe pointing outward or twisting while walking. If left untreated, the condition can worsen and cause pain in the spine and pelvis due to foot imbalance.
What are the treatment options for different types of bunions?
Bunion with a normal arch
If the arch is normal, the issue may lie with the shoes themselves. Avoiding high heels and opting for wide-footed shoes can help prevent further progression of the bunion.
Bunion with a low arch
When the foot shape is already distorted or there is an underlying foot imbalance, changing shoes alone will not stop the progression of the bunion. Foot orthosis is recommended to address the symptoms of hallux valgus (bunion) in this case.
To prevent early bunion deformity, the most important treatment is the use of foot orthosis. For deformations measuring 40 degrees or less, the progression of bunion transformation can be prevented solely through foot orthosis and exercise therapy, without the need for surgery. Additionally, exercises to strengthen the foot and calf muscles, as well as avoiding habits that exacerbate the deformity, can effectively prevent further bunion progression.
Type 3. Habitual Sprain
Common symptoms of a habitual sprain include pain, swelling in the ankle ligament, and gait disturbances. In severe cases, immediate swelling accompanied by a “popping” sound at the ankle may indicate significant damage. After a day or two, bruising may develop around the entire ankle, extending beyond the outer area in the case of a severe sprain.
Different types of ankle sprains can occur:
Lateral ligament ankle sprain
Approximately 85% of ankle sprains involve the lateral ligaments of the ankle.
Digital tibiofibular ligament ankle sprain
In around 5% of cases, the ligament connecting the tibia and fibula is damaged, which often requires a longer recovery period.
Medial ligament ankle sprain
Ankle medial ligament damage is less common. Individuals with flat feet or a low foot arch may experience chronic medial pain.
The goal of sprain treatment is to prevent chronic pain and instability. Even a mild sprain can become recurring if not adequately treated. Severe sprains can result in chronic pain, ankle instability, and even arthritis. Active and continuous treatment is necessary to manage the condition effectively.
Type 4. Tarsal Tunnel Syndrome
Tarsal tunnel syndrome refers to the numbness and tingling sensation in the soles of the feet caused by pressure on the plantar nerves as they pass through the tarsal tunnel. The tarsal tunnel is the area between the inner ankle and the heel, where most of the tendons, nerves, and blood vessels responsible for foot movement and nourishment are located. When the nerve passing through this tunnel becomes compressed, symptoms of tarsal tunnel syndrome can occur.
What are the symptoms of tarsal tunnel syndrome?
Dull pain, either hot or of a low intensity, in the soles of the feet.
Pain that may radiate down towards the sole or extend into the legs.
Symptoms that worsen with activity and improve with rest.
Pain or sensitivity upon touching specific areas along the path of the affected nerve.
Numbness in the feet and weakness leading to toe deformities when symptoms worsen.
What are the causes of nerve compression in the tarsal tunnel?
Ankle sprains, fractures, or bruises that result in damage to the area.
Low foot arches, which can contribute to the compression of the nerves.
Sudden and excessive physical activity.
Rapid weight gain or prolonged periods of standing.
High arches in individuals who are prone to ankle sprains.
Treatment options for tarsal tunnel syndrome involve the use of foot orthotics to correct the foot arch. Acupuncture can also provide relief by alleviating nerve entrapment. Re-memory therapy, focusing on muscle and fascia correction for foot and calf muscle recovery, can offer fast and effective symptom relief.
With appropriate treatment, symptoms of tarsal tunnel syndrome typically improve within 3 to 6 weeks.
Type 5. Sinus Tarsi Syndrome
Sinus tarsi syndrome is commonly caused by traumatic injuries to the ankle or foot, such as ankle sprains, as well as overuse from repetitive activities like standing or walking. Individuals with flat feet or a low foot arch are more prone to developing sinus tarsi syndrome. This is because flat feet or low arches lead to increased ankle movement and instability, which can result in the overstretching or tearing of ligaments, leading to inflammation. If left untreated, this condition can become chronic and may eventually contribute to the development of degenerative arthritis.
What are the symptoms of sinus tarsi syndrome?
Soreness in the ankles, even after minimal activity or light walking.
A feeling of instability in the ankles, as if they are at risk of spraining.
Lack of recovery following an ankle sprain, with symptoms persisting chronically.
Sinus tarsi syndrome is commonly associated with flat feet or low foot arches. If left untreated and allowed to become chronic, it can result in degenerative arthritis in the subtalar joint. Early treatment is crucial to prevent further complications.
When addressing the functional imbalances that can lead to conditions like Morton’s neuromas, it is important to perform an accurate examination of the foot shape. Precise foot orthotics should be used to provide effective treatment. Utilizing appropriate foot orthotics can yield excellent treatment outcomes.
Type 6. Achilles Tendinitis
What causes Achilles tendinitis?
Achilles tendinitis is inflammation of the Achilles tendon, which is a strong fibrous band connecting the calf muscles to the heel bone.
Several factors can contribute to the development of Achilles tendinitis:
Tight and stiff calf muscles
When the calf muscles are excessively tight and lack flexibility, it increases tension on the Achilles tendon, making it more prone to tears and damage.
Foot deformities
Flat feet or low foot arches can increase tension on the Achilles tendon, leading to Achilles tendinitis. Treatment for foot deformities often involves the use of foot orthotics to address the foot’s alignment and support the calf muscles.
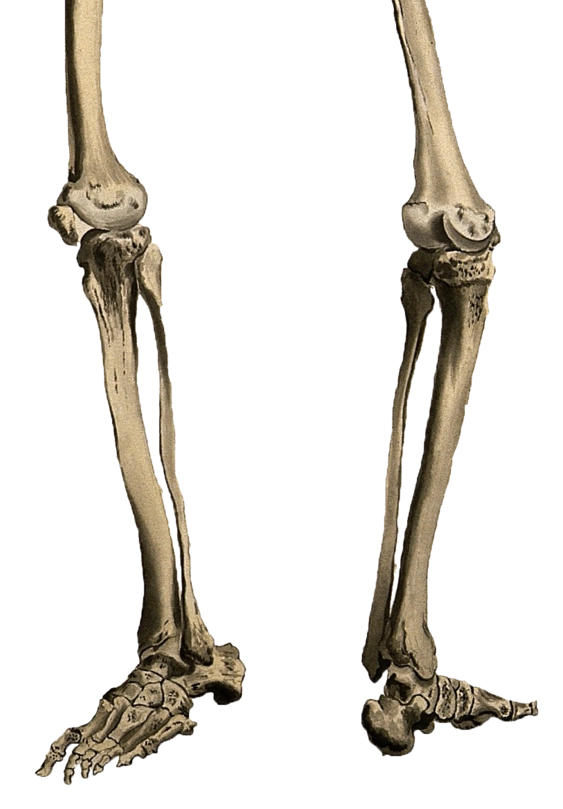
Leg length discrepancy
When there is a significant difference in leg length, it can place uneven stress on one Achilles tendon, making it susceptible to damage. Persistent strain and imbalance can lead to chronic Achilles tendinitis.
Heel pain due to footwear
Friction caused by ill-fitting or improper shoes can result in pain and irritation in the upper part of the heel. If there has been a recent change in footwear, it may be a contributing factor to the pain.
What are the symptoms of Achilles tendonitis?
Achilles tendon pain in the heel area following intense exercise or movement.
Swelling around the ankle, limiting exercise capabilities.
Morning heel pain and discomfort when first stepping on the feet.
Calf cramps.
Tingling, pain, and a burning sensation in the toes.
Type 7. Morton’s Neuroma
What is Morton’s neuroma?
Morton’s neuroma is characterized by symptoms of pain, tingling, and burning in the toes. It is caused by repeated compression and friction of the nerves between the toe bones.
Several factors can contribute to the development of Morton’s neuroma:
Wearing high-heeled or narrow shoes
Footwear that compresses the toes, such as high heels or shoes with a narrow toe box, can increase the risk of developing Morton’s neuroma.
Foot deformities:
Certain foot deformities, such as high arches or flat feet, can put additional pressure on the nerves and contribute to the development of Morton’s neuroma.
Stiffness of the big toe
When the big toe does not have sufficient mobility and flexibility, it can lead to increased stress on the other toes, potentially causing Morton’s neuroma.
Wide gap between the heads of the metatarsal bones
A low transverse arch of the foot can result in a wider gap between the heads of the metatarsal bones, which can contribute to the compression of nerves and the development of Morton’s neuroma.
What are the symptoms of Morton’s neuroma?
Soreness and tingling in the toes, particularly between the 3rd and 4th toes.
Symptoms that worsen when wearing shoes, with pain alleviating or disappearing when shoes are removed.
Pain or discomfort in the front part of the foot.
Aggravation of symptoms when wearing pointed shoes or high heels.
Morton’s neuroma can be effectively treated through various methods, including foot support, orthotics, and re-memory therapy.
